Jamie Perry, DTMH 2017
I write this following a bittersweet time for many of us, with the 3 month Diploma of Tropical Medicine and Hygiene having now finished, goodbyes having been said (over not one, nor two, but three different farewell evenings) and the prospect of what I think is referred to as “real life” dawning perilously close on the horizon. I’ve even made a laptop wallpaper out of mosquito pictures to prolong the tropical geekiness for longer (in case anyone wonders if I’m joking about this, here’s a screenshot below. I’m sadly not).

Several of us from the course stayed on to do another course, which is the subject of today’s blog. This is the “EOC” course, referring to Emergency (or Essential) Obstetrics Care, particularly in focussing in low resource settings.
Chatting to the other course attendees, several had either a past or future link with LSTM, either having previously done one of the other medical (e.g. DTMH) or nursing (e.g. DTN) courses or being about to start one. However what was clear is that for most attendees, with or without an LSTM link, their reason for wanting to be on this course on particular was to gain skills which could be applied to a low resource setting, and this was a recurrent theme of the teaching.
I was impressed by the teaching staff’s mix of skills and prior experiences. On this occasion there were several midwives, consultant obstetricians and an obstetric anaesthetist. They were all very familiar how in practice to work in low resource settings, and the course in its current form now goes to such settings (with one of the faculty telling me she’s already been to South East Asia and Sub-Saharan Africa this year with the course).
The main course was over 3 full days, with an optional extra half day which I’d recommend attending if practical, as it sets up the rest of the course quite well (ABCDE approach particularly focussed on obstetrics, and normal labour).
The usual structure is a 20 minute lecture on a topic (e.g. post-partum haemorrhage) followed by four 15-20 minute stations in small groups (up to 8 people) which are usually more hands on. These will be led by two faculty members, so for some skills-based things there is scope to split into two groups of 4 to get more hands-on time, although often particularly for a more ABCDE acute illness station we stayed as one group and discussed the points together.
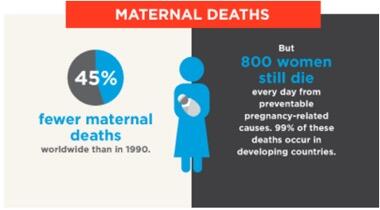
Regarding the course content, the full list is on the link I posted earlier so I won’t repeat it, but it’s worth providing some context and comment about it. The question of interest is which obstetric skills and resources are “essential” if low and middle income countries in particular are to further reduce maternal mortality ratios (for more on these targets click here). The course outlines 7 things that all “basic” obstetric facilities should be able to offer to achieve this aim, and a further 2 that a “comprehensive” obstetric facility adds. As of 2009, WHO’s recommendation is that each population of 500,000 should have at least 4 basic and 1 comprehensive facility.