Background
Skilled midwives are essential in contributing to a reduction in maternal and newborn mortality and improving access to quality care across the continuum of antenatal, birth and postpartum periods. When supported by interdisciplinary teams and working within an enabling environment, midwives can deliver ~ 90% of essential sexual, reproductive, maternal, newborn and adolescent health interventions and save up to 4.5 million mothers and newborns annually by 2035. However, evidence shows that midwifery education and training in low- and middle-income countries (LMICs) remains grossly under-invested with a deficient and largely didactic curriculum, inadequate teaching resources and lack ofor insufficiently trained midwifery educators leading to less skilled graduates. Our earlier study suggests high variation in the baseline knowledge and skills of maternity care providers in sub-Saharan Africa countries, this may be due to deficient pre-service training curriculum.
Global standards for midwifery education
In 2021, the International Confederation of Midwives (ICM) updated their standards for midwifery education focusing on programme governance, faculty, students, curriculum, resources and quality improvement. On midwifery programme and curriculum review and implementation, at least 50 percent of midwifery education should be practice-based and provide experience in clinical and community settings, in direct contact with women and newborns. Midwifery educators must have core competencies by WHO required to teach a competent-based curriculum to develop and improve the professional skills among students. Despite this requirement, inadequate clinical areas for clinical practice hamper the achievement of this essential component causing students to graduate with outdated practices. Therefore, there is need to provide a robust system to enable students to learn and develop their clinical and professional skills supported by competent educators.
Liverpool School of Tropical Medicine (LSTM) supports implementation of pre-service interventions that focus on improving the quality of pre-service midwifery and reproductive health education and training in Kenya, through support from Johnson and Johnson Foundation, FCDO Kenya and in collaboration with the Alliance for Improving Midwifery Education lead by UNFPA Sexual and Reproductive Health Branch, Technical Division.
The third of four Knowledge Management and Learning (KML) events in the final year of the FCDO Kenya MNH programme, was hosted by Vihiga County on 1st and 2nd November 2022. The event brought together stakeholders from the Ministry of Health, nursing and midwifery training regulator – Nursing Council of Kenya (NCK), Kenya Medical Training College (KMTC), Midwives Association of Kenya, Clinical Officers Council, midwifery training universities, implementing and neighbouring counties, and development partners in Kenya. The aim of the event was to share lessons learnt in the implementation of the MNH programme with a view of enhancing sustainability measures that will be adopted for implementation beyond the programme. For the pre-service component of the programme, this provided an opportunity to develop an exit strategy to ensure that the gains accrued from the mid-level KMTC’s midwifery and clinical medicine (reproductive health) faculty development interventions are scaled and sustained beyond the programme.
Preliminary results from an evaluation of the effectiveness of an updated midwifery curriculum in Kenya: a cluster randomised controlled trial
A cluster randomised controlled trial (https://doi.org/10.1186/ISRCTN14203188) in 20 midwifery colleges (12 intervention and 8 control), comprising 72 midwifery educators was conducted. Educators in both arms received training in teaching skills and selected EmONC skills, with those in the intervention arm receiving additional support mentoring every three months after training for 12 months. Results at the end of the mentoring intervention showed that before training, the mean knowledge scores for intervention and control arms were 63.3% and 59.0% respectively. Immediately after the training, mean knowledge scores improved to 75.4% (p=0.006) in the intervention and 70.3% (p=0.056) in the control arm. Within each arm there were no statistically significant differences from the immediate post training scores at each of the subsequent assessments. Baseline mean scores of observed teaching skills for intervention and control arm was 68.9% vs 68.8%. At endline, there was a 20.4% (p=0.003) and 3.6% (p=0.634) improvement in the intervention and control arms respectively. The mean performance scores for students in the common midwifery promotional examinations were similar for the two arms in the baseline class (54.8% vs 59.0%). In the two subsequent class intakes, the mean performance scores improved by 7% (p=0.013) and 6.1% (p=0.035) in the intervention arm with no improvements in the control arm (p>0.05). In conclusion, training improved knowledge and teaching skills of educators and mentoring of educators over time improved their teaching skills and students’ performance.
Action plan to sustain the gains achieved
Kenya’s Ministry of Health’s Pre-service taskforce stakeholders led by the KMTC identified key priorities to scale and developed an action plan of investments to be implemented to sustain the midwifery educators’ faculty development and implementation of a competency-based midwifery curriculum.
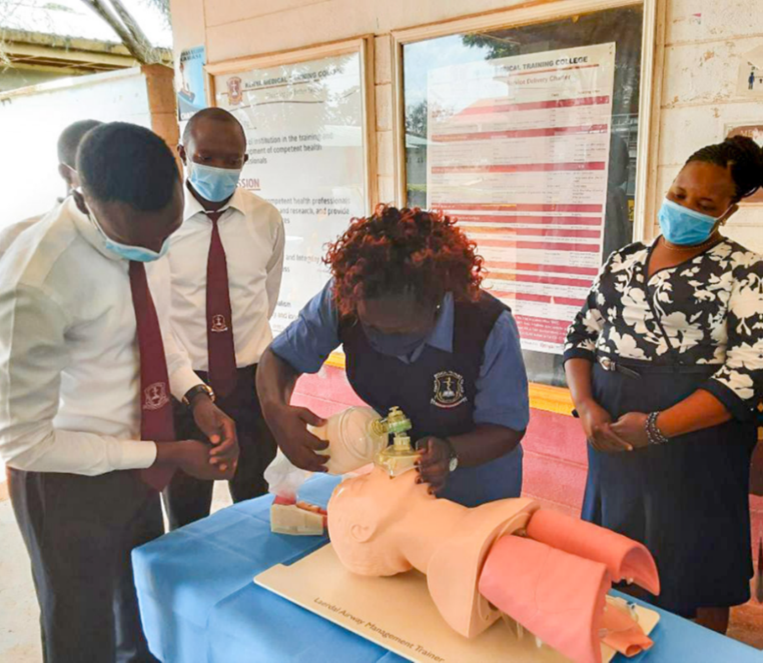
1. Maintenance of skills lab EmONC training equipment
The equipped KMTCs require a designated staff to regularly ensure that the skills lab training equipment are well maintained by performing regular inventory audits and functionality checks of the equipment. Efforts should be made by each KMTC campus to support the skills lab equipment maintenance and functionality.
2. Capacity strengthening of midwifery educators on EmONC and teaching skills
Over 300 midwifery and clinical officers (reproductive health specialty) educators from KMTC have been trained on EmONC and have the capacity to deliver the EmONC-enhanced curriculum. Peer teaching and support is a key strategy that promotes confidence, autonomy, communication, collaboration and teamwork among educators in teaching, students’ assessments and providing effective feedback. Secondly, lecturers from the two departments (midwifery and clinical medicine) to organize for team teaching for practical skills as per curriculum requirements and where human resource is insufficient, campuses to engage trained county staff using the KMTC hiring staff policy for the hours required.
3. Mentoring of midwifery educators on EmONC and teaching skills
Through the Office of the Academic Registrar, KMTC to strengthen regional mentorship centres (previously clustered in the traditional eight provinces in the country) where national master trainer educators from KMTC will on regular structured basis – twice a year, offer refresher training skills to their colleagues.
4. Student facilitators
For continuity of practice, midwifery educators should identify potential highly motivated student facilitators (either from same cohort or upper cohorts) to support mentoring their colleagues (students peer mentoring). Evidence shows that the practice of using student peers incidentally or purposefully in the clinical education of apprentice or undergraduate health science students can increase student's confidence in clinical practice and improve learning in the psychomotor and cognitive domains.
5. Continuous professional development
Continuous professional development (CPD) offers opportunities for educators to sustain and improve their knowledge and skills in theoretical and practical skill teaching. With the established midwifery educator CPD program, KMTC to facilitate their educators to access the CPD opportunities in the established hubs at Nairobi and Kakamega KMTCs to enhance their knowledge and skills competencies.
Conclusion
The capacity strengthening interventions improved the midwifery educators’ competencies in delivering the updated competency-based curriculum enhanced with EmONC as recommended by ICM, WHO, UNFPA and other leading stakeholders in maternal and newborn health. The KMTC focuses on scaling and sustaining the high-impact sustainable interventions to improve the quality of midwifery education through a competency-based curriculum, skilled faculty, equipped skills labs for skills training and motivated students for a resilient midwifery workforce. This strategy is a pathway to ensuring high quality skilled health personnel at graduation in LMICs for improved maternal and newborn health and outcomes.