
Tuberculosis (TB) has affected humankind for millennia. Each year, TB continues to cause 10 million people to fall ill, 1.5 million people to die, and countless families to suffer hardship. Since 2020, the Covid-19 pandemic has dominated our lives and overshadowed the ongoing global public health emergency that TB represents.
On World TB Day, 24th March 2022, we follow the journey of a TB-affected person from illness to cure, to shine a light on TB and the key advances being made in TB research, policy and advocacy.
A troublesome cough
TB often starts with a cough. But coughs are common, especially in these Covid times, and may be tolerated, ignored or misdiagnosed as a chest infection, sometimes multiple times. Despite the cough, life goes on because it must: the need to work, to earn, to gain education, to care for dependents. But the cough persists and may start to be accompanied by sweats, fever, and weight loss, among other symptoms. Many people with TB have had their symptoms for months before TB is finally diagnosed and treated.
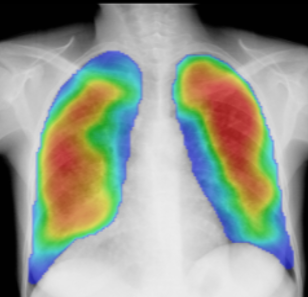
digital chest x-ray can reduce delays to starting TB treatment [1].TB used to be diagnosed by looking at samples of phlegm down a microscope. More recently, the first line TB test in most TB endemic areas is a molecular test, similar to the Covid-19 “PCRs” that we are now all too familiar with, that identifies TB bacterial DNA in the sample. Molecular tests detect more cases first time than the traditional microscope-based tests. They also have the advantage of being able to identify if the TB infection is drug-resistant. This is important because it helps healthcare professionals know which TB drugs to use and not use and to try to avoid transmission of drug-resistant TB (see below). Some people may be diagnosed with TB by chest x-ray. A recent LSTM-led study in Malawi suggested that screening people with cough for TB using digital chest x-ray can reduce delays to starting TB treatment [1].
Figure 1: A digital chest X-ray showing areas suggestive of tuberculosis (highlighted in orange and red) as identified by computer-aided detection (CAD). Source https://www.delft.care/cad4tb/. CAD4TB software is one of several commercially-available CAD softwares.
Finding the missing millions
Of the 10 million people who were ill with TB in 2020, the WHO estimates that 4 million were never diagnosed or treated. The reasons for this are complex and include lack of access to healthcare, poor infrastructure, inadequate TB diagnostic or treatment facilities, or – as mentioned above - misdiagnosis. To find the missing millions, we need more active case finding to take screening and diagnosis to communities, especially those at highest risk.
TB treatment
But even for those who are diagnosed with TB and treated, their journey is far from over. For decades, standard TB treatment has been 6 months of daily medications. This treatment requires multiple pills per day and some people experience significant side effects that make it harder to keep taking the medicines. Thankfully, this year, there have been some major breakthroughs on this front with two trials showing a new four-month treatment regimen to be as effective as the standard 6-month course for some forms of TB, in adults and children [2,3]. Despite this progress, there are still barriers to transforming these findings into policy change and making a 4-month regimen a reality for health systems and people with TB.
Stigma and costs of TB
As with other illnesses, such as Covid-19 and HIV, stigma is a key challenge facing people with TB. Sadly, stigma can come from many quarters including family, neighbours, healthcare workers, and even self-stigma of the person affected. This can impact upon quality of life and mental wellbeing. Economically, people with TB may not be able to work due to illness, having to go to healthcare facilities or clinics daily to collect and be watched taking their medicines, or losing their job. One in two TB affected households globally experience catastrophic costs of TB, which reduce the chances of TB treatment success and push TB-affected households deeper into poverty [4,5].
Drug resistant TB
Drug-resistant TB is one of the leading killers due to antimicrobial resistance, globally [6]. WHO’s Global TB Report suggests that 3-4% of all TB cases diagnosed are resistant to multiple TB drugs (multidrug resistant TB or MDR-TB) and, in some parts of the world, this proportion is much higher. MDR-TB does not respond to two key frontline TB medicines, rifampicin and isoniazid. People with MDR-TB have traditionally required much longer TB treatment regimens with at least 18 months of multiple medications. As a recent study between LSTM and the Sierra Leone MDR-TB Programme showed, this treatment is associated with severe side effects and people with MDR-TB are less likely to be cured than those without resistant variants [7]. The good news is that there has been some progress on this front too. Two studies of regimens including new oral TB drugs (ZeNix and TB-Practecal) have shown good results that give hope that shorter regimens with fewer medications are on the horizon to successfully treat drug-resistant TB.
Preventing TB
What about transmission of TB to contacts of people with TB? Are contact tracing and self-isolation, tools now familiar from attempts to control COVID-19, relevant to prevent TB transmission? The answer is yes. Not unlike SARS-CoV-2, the bacteria that causes TB, Mycobacterium tuberculosis, is transmitted from person-to-person by airborne particles from people with lung TB through, for example, coughing. Those in close contact such as in a household or workspace, especially when ventilation is poor, are most likely to be affected. There are multiple ways to try and prevent TB among contacts. First, there is prompt TB diagnosis and treatment to reduce the time that contacts are exposed to an infectious person with symptoms. Work of the LIGHT consortium in Kenya, Malawi, Nigeria, Uganda and UK, is helping to remove barriers to accessing TB care, particularly those experienced by men who are less likely to come forward for TB testing. Second, people exposed to TB can be screened for TB infection and disease. For those who have evidence of infection but no symptoms or signs of TB disease – sometimes called latent TB infection - there are preventive therapies available to stop them going on to develop TB. Third, as we have all become familiar with, respiratory precautions such as face masks can help to protect people from transmission of TB. However, while all of the above are the ideal for TB care and prevention, they require resource allocation, which is not universally available, especially in the highest TB burden settings.
TB treatment success
Back to the TB journey - the cough that eventually led to TB diagnosis and treatment – we ask, “will the TB treatment work”? WHO data suggests that, overall, 86% patients with drug-sensitive forms of TB are treated successfully (complete treatment or proven cured). However, for many, the journey still does not stop at cure. Many “successfully-treated” people are left with scars from their TB illness. These scars can be both physical, such as chronic lung disease [8, 9], and psychological, such as anxiety or low mood. The International Union against Tuberculosis and Lung Disease have recognised this and published the first set of standards for clinical management of patients with lung disease post-TB. Research identifying damaging immune responses to TB bacteria is starting to identify potential candidate treatments that may improve long term outcomes from TB, pending further study in clinical trials.
Vaccines old and new
Vaccination has been heralded as the solution to the Covid-19 pandemic. What about vaccines for TB? There is a vaccine for TB called “BCG” which has been around for more than 100 years. BCG is helpful to prevent severe forms of childhood TB if given to infants but does not effectively prevent infectious forms of TB in adults. There is an effort to generate new TB vaccines but a key hurdle is determining exactly what constitutes an effective immune response to TB. Too little immunity and there is a risk of life-threatening infection, too much immunity and there is risk of a damaging immune response that causes disease.
Can the world now learn lessons from this new global Covid-19 pandemic to apply to the long-standing global TB pandemic? We believe it can and should [10, 11]. Reminding those with power and influence that TB health workers, hospitals, labs and TB care platforms were instrumental in the fight against Covid-19 and that TB can and will affect them if nothing is done, may help combat indifference. Ensuring no one with TB is left behind, is essential.
On World TB Day 2022, let’s put TB in the spotlight and keep people with TB at the very centre of it all.
Invest to End TB – Save lives!
References
1. MacPherson P, Webb EL, Kamchedzera W, Joekes E, Mjoli G, Lalloo DG, Divala TH, Choko AT, Burke RM, Maheswaran H, Pai M, Squire SB, Nliwasa M, Corbett EL. Computer-aided X-ray screening for tuberculosis and HIV testing among adults with cough in Malawi (the PROSPECT study): A randomised trial and cost-effectiveness analysis. PLoS Med. 2021 Sep 9;18(9):e1003752. doi: 10.1371/journal.pmed.1003752. PMID: 34499665; PMCID: PMC8459969.
2. Dorman SE, Nahid P, Kurbatova EV, Phillips PPJ, Bryant K, Dooley KE, Engle M, Goldberg SV, Phan HTT, Hakim J, Johnson JL, Lourens M, Martinson NA, Muzanyi G, Narunsky K, Nerette S, Nguyen NV, Pham TH, Pierre S, Purfield AE, Samaneka W, Savic RM, Sanne I, Scott NA, Shenje J, Sizemore E, Vernon A, Waja Z, Weiner M, Swindells S, Chaisson RE; AIDS Clinical Trials Group; Tuberculosis Trials Consortium. Four-Month Rifapentine Regimens with or without Moxifloxacin for Tuberculosis. N Engl J Med. 2021 May 6;384(18):1705-1718. doi: 10.1056/NEJMoa2033400. PMID: 33951360; PMCID: PMC8282329.
3. Turkova A, Wills GH, Wobudeya E, Chabala C, Palmer M, Kinikar A, Hissar S, Choo L, Musoke P, Mulenga V, Mave V, Joseph B, LeBeau K, Thomason MJ, Mboizi RB, Kapasa M, van der Zalm MM, Raichur P, Bhavani PK, McIlleron H, Demers AM, Aarnoutse R, Love-Koh J, Seddon JA, Welch SB, Graham SM, Hesseling AC, Gibb DM, Crook AM; SHINE Trial Team. Shorter Treatment for Nonsevere Tuberculosis in African and Indian Children. N Engl J Med. 2022 Mar 10;386(10):911-922. doi: 10.1056/NEJMoa2104535. PMID: 35263517; PMCID: PMC7612496.
4. Wingfield T, Boccia D, Tovar M, Gavino A, Zevallos K, Montoya R, Lönnroth K, Evans CA. Defining catastrophic costs and comparing their importance for adverse tuberculosis outcome with multi-drug resistance: a prospective cohort study, Peru. PLoS Med. 2014 Jul 15;11(7):e1001675. doi: 10.1371/journal.pmed.1001675. PMID: 25025331; PMCID: PMC4098993.
5. Wingfield T, Tovar MA, Datta S, Saunders MJ, Evans CA. Addressing social determinants to end tuberculosis. Lancet. 2018 Mar 24;391(10126):1129-1132. doi: 10.1016/S0140-6736(18)30484-7. PMID: 29595481; PMCID: PMC7611140.
6. Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022 Feb 12;399(10325):629-655. doi: 10.1016/S0140-6736(21)02724-0. Epub 2022 Jan 19. PMID: 35065702; PMCID: PMC8841637.
7. Kamara RF, Saunders MJ, Sahr F, Losa-Garcia JE, Foray L, Davies G, Wingfield T. Social and health factors associated with adverse treatment outcomes among people with multidrug-resistant tuberculosis in Sierra Leone: a national, retrospective cohort study. Lancet Glob Health. 2022 Apr;10(4):e543-e554. doi: 10.1016/S2214-109X(22)00004-3. PMID: 35303463.
8. Meghji J, Lesosky M, Joekes E, Banda P, Rylance J, Gordon S, Jacob J, Zonderland H, MacPherson P, Corbett EL, Mortimer K, Squire SB. Patient outcomes associated with post-tuberculosis lung damage in Malawi: a prospective cohort study. Thorax. 2020 Mar;75(3):269-278. doi: 10.1136/thoraxjnl-2019-213808. Epub 2020 Feb 26.PMID: 32102951 Free PMC article.
9. Meghji J, Gregorius S, Madan J, Chitimbe F, Thomson R, Rylance J, Banda NP, Gordon SB, Corbett EL, Mortimer K, Squire SB. The long term effect of pulmonary tuberculosis on income and employment in a low income, urban setting. Thorax. 2021 Apr;76(4):387-395. doi: 10.1136/thoraxjnl-2020-215338. Epub 2020 Dec 18.PMID: 33443228
10. Wingfield T, Karmadwala F, MacPherson P, Millington KA, Walker NF, Cuevas LE, Squire SB. Challenges and opportunities to end tuberculosis in the COVID-19 era. Lancet Respir Med. 2021 Jun;9(6):556-558. doi: 10.1016/S2213-2600(21)00161-2. Epub 2021 Mar 24. PMID: 33773121; PMCID: PMC7988354.
11. Pai M, Kasaeva T, Swaminathan S. Covid-19's Devastating Effect on Tuberculosis Care - A Path to Recovery. N Engl J Med. 2022 Jan 5. doi: 10.1056/NEJMp2118145. Epub ahead of print. PMID: 34986295.
Links
Click on the embedded links for further information. The following links are for related organisations, global and national action plans for TB and ideas about how you can take action!
- TB Alert : https://www.tbalert.org
- Treatment Action Group (TAG): https://www.treatmentactiongroup.org
- Policy paper. Tuberculosis (TB): action plan for England: https://www.gov.uk/government/publications/tuberculosis-tb-action-plan-for-england
- UK Academics & Professionals to End TB https://ukaptb.org/
- WHO Factsheet on TB https://www.who.int/news-room/fact-sheets/detail/tuberculosis
- The WHO Global Tuberculosis Programme https://www.who.int/teams/global-tuberculosis-programme/the-end-tb-strategy