
Authors
Onesmus Muchemi, Technical Officer – Liverpool School of Tropical Medicine (LSTM) Kenya
Fatuma Iman –Reproductive Health Coordinator, Garissa County, (Kenya)
Martin Eyinda, Technical Officer – Liverpool School of Tropical Medicine (LSTM) Kenya
Irene Nyaoke, Senior Technical Officer - Liverpool School of Tropical Medicine (LSTM) Kenya
Rael Mutai, Regional Technical Advisor- Liverpool School of Tropical Medicine (LSTM) Kenya
Lucy Nyaga, Country Director- Liverpool School of Tropical Medicine (LSTM) Kenya
Charles Ameh, Professor Global Health, Head Emergency Obstetric and Quality of Care Unit, Liverpool School of Tropical Medicine (LSTM) United Kingdom.
Iftin Sub-County Hospital (SCH) in Garissa County, is one of 61 health facilities in Kenya supported by LSTM with a grant from the Global Fund to implement quality improvement in integrated antenatal and postnatal care. The program is implemented in collaboration with Garissa County health department and aims at strengthening the capacity of health care providers in providing quality maternal and newborn healthcare.
Garissa county has a high burden of maternal mortality, with a maternal mortality ratio (MMR) estimated to be 641/100,000 live births. This compares to a national average of 362/100,000 live births (KNBS, 2009). Iftin SCH provides maternal and newborn health services, with an average of 50 mothers giving birth each month, 90 mothers attending for ANC booking, and 250 revisits. In the month of March 2023, a meeting was held with Iftin SCH staff, to allow Mr Feisal Ahmed, the health worker who was trained on quality improvement to give feedback after the training. In the meeting, Feisal explained the importance of quality improvement and application of standards-based audit (St-BA) was highlighted as a strategy for improving the quality of care in antenatal and postnatal services. Following the feedback, a facility quality improvement team (QIT) was constituted, consisting of six members.
In April 2023, the QIT started the implementation of a St-BA cycle by listing and prioritising the problems affecting the maternal new-born health services. The problems identified included, lack of maternity inpatient files, lack of back-up generator, unavailability of ambulance for referral, severe shortage of staff, lack of privacy for patients, and inadequate assessment of postnatal mothers in the 24 hours prior to discharge. Based on the prioritisation, the team identified inadequate postnatal assessment and lack of inpatient files as being in most urgent need of action, as they could negatively impact the lives and wellbeing of mothers and newborns. The problems link to Ministry of Health, Maternal and Newborn Health (MNH) quality standards 2 and 3, with the following associated quality statements:
- All women are assessed in the first 24 hours after birth by a skilled healthcare provider before discharge from a healthcare facility.
- Every woman and new-born have a complete, accurate and standardised medical record during the antenatal period, labour, childbirth, and the early postnatal period.
The actions proposed to address the two standards were to ensure that all postnatal mothers are assessed prior to discharge, and that adequate stocks of maternity files were available.
The QIT requested the allocation of funds from the hospital budget by the hospital management, so that these issues could be resolved.
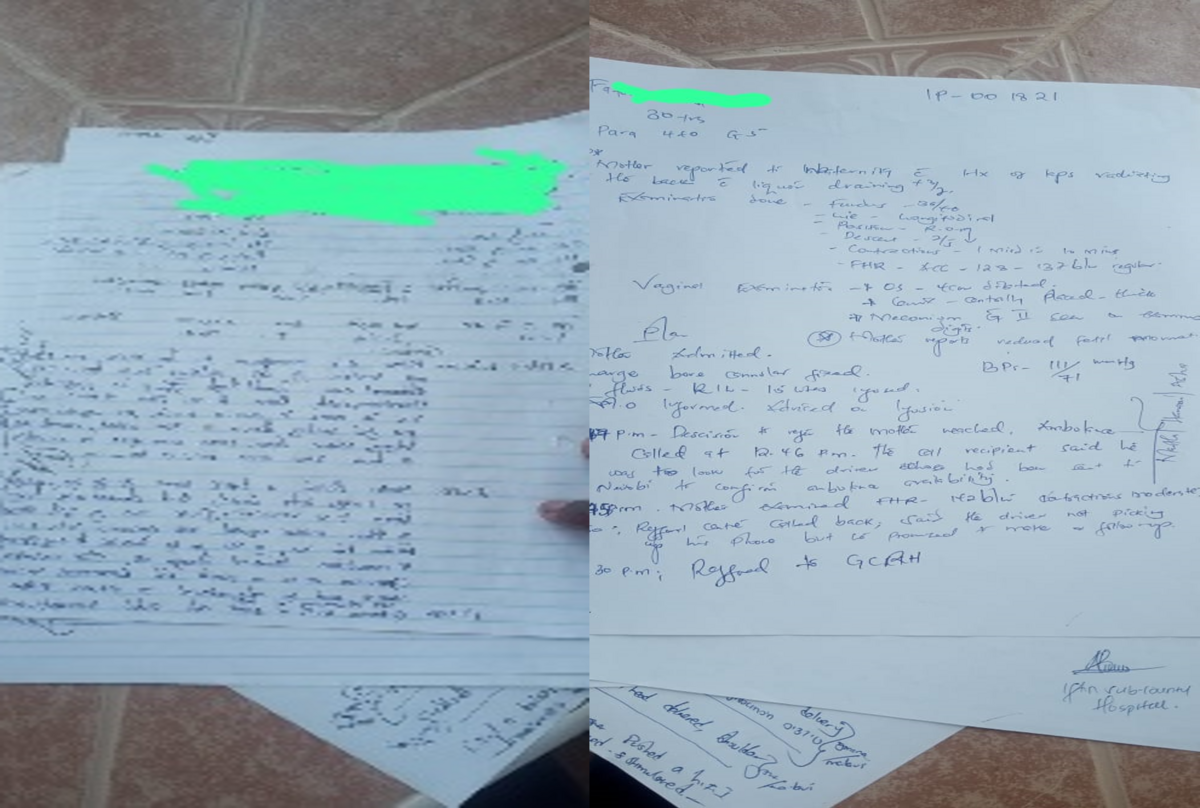
Iftin Sub-County Hospital started providing maternity services in the year 2000. Since then, there has not been proper documentation of maternal and newborn health services. Care provided was documented on pieces of plain paper which were pinned together to make patient case notes. These improvised notes were prone to falling apart, contributing to loss of essential documentation of care. The lack of partographs also contributed to poor management and decision making for mothers in labour, resulting in unnecessary interventions and referrals. It is difficult to trace any records of care for individual mothers and babies during the period 2000-2023.
A midwife working in maternity, who is also a member of the facility QIT made the following comment:
“We did not have patient files for a long time, and we felt it was not right. There was no partograph and we could not monitor the progress of labour. We referred pregnant mothers without knowing the status of labour. So, we could refer just because we felt we had stayed with the mother for long. We documented care on pieces of paper, where we wrote a short history of the mother, delivery, and postnatal report. That was it. Once care was provided, the pieces of paper would just be left lying on the table. With time, the papers would just fall off, and the cleaner would pick them up and dispose them away.
Ideally, proper filing promotes quality care, information generation by health workers, and after discharge of the patient the document is taken to the records department for storage. So, in our case, there is hardly any record in storage before April 2023 the time we implemented quality improvement”. (Midwife, maternity)
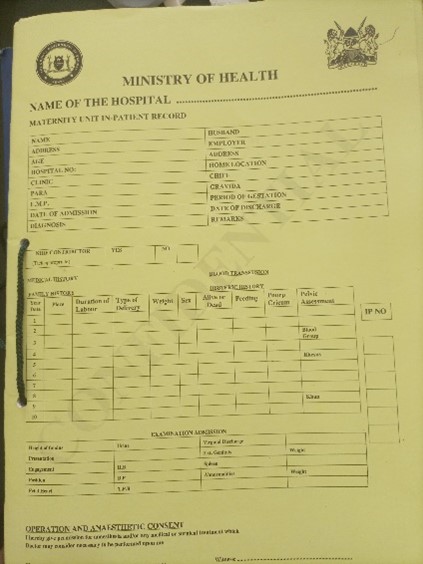
The QIT reported their concern on the absence of standardised medical records for the mothers during labour and after birth, and the impact it had on the quality of care. However, at that time the feedback from hospital management was that there were no funds to support the initiative. The QIT persisted however, and subsequently, with the support of the nursing officer in charge, and when a member of County Health Management Team (CHMT) came for a supportive supervision visit, they were informed of lack of documentation at the maternity unit, and the standard they had set up to close the gap. This was discussed with the Medical Superintendent, who was eventually able to secure funds from the hospital budget and printed some copies of case files. These were only expected to last a short period of time, so the nursing officer in charge took the initiative and visited the Sub-County offices where she found 100 new files that had been awaiting distribution to the facility.
As a result of this intervention, work has become easier, and records are kept up to date. Quality of care has improved because health care providers have better access to clinical information. It is possible to document the medical history, and the care being provided to the mother and the baby until discharge. After care is over and the client is discharged, the case file is preserved by the records department. The health records officer in the hospital made the following statement:
“Before, there were no patient files. Patient notes were written on pieces of plain papers, and sometimes even the plain papers were not available. The written papers were not submitted to the records department, they remained in maternity. There were no notes, no partographs, there was nothing to file. Now, filing is much better. However, my current problem is lack of a filing area. When the case notes come from maternity, I store them in boxes. I have reported this matter to the hospital management for intervention.” (Health Records Officer)
The QIT plans to conduct a second measurement to evaluate the achievement of their targets against the quality standard. The facility has adequate stocks of files to last them for approximately two months and the nurse manager plans to include the procurement of files in the facility budget. This will be the only way to make the change impactful and sustainable.