
Authors
Irene Nyaoke, Senior Technical Officer - Liverpool School of Tropical Medicine (LSTM) Kenya
Rael Mutai, Regional Technical Advisor- Liverpool School of Tropical Medicine (LSTM) Kenya
Helen Allott –Technical Specialist - Liverpool School of Tropical Medicine (LSTM) United Kingdom
Lucy Nyaga, Country Director- Liverpool School of Tropical Medicine (LSTM) Kenya
Charles Ameh, Professor Global Health, Head Department International Public Health, Liverpool School of Tropical Medicine (LSTM) United Kingdom
Competence-based training in Emergency Obstetric and Neonatal Care (EmONC) can significantly improve healthcare provider knowledge, skills and clinical practice thus contributing to ending preventable maternal mortality. However, without post training support, skills and knowledge gained tends to erode over time.
Ministry of Health (MoH) in Kenya has identified EmONC training and mentorship as a strategy to enable healthcare providers not only advance, but also utilise and cascade their knowledge, skills, attitudes, and competencies using a standardised facility-based mentorship approach. A national EmONC training and mentoring package was co-created with support from Liverpool School of Tropical Medicine (LSTM). After the launch of the package in June 2022, LSTM has disseminated and built capacity of health workers in several counties in Kenya on the package. The LSTM Led, capacity-strengthening project in Nairobi County, is in partnership with the county health department and funded by United Nations Population Fund (UNFPA).
Zero maternal and neonatal deaths in Nairobi! that is what I desire to see; let us saturate the county with these life-saving skills ...
Dr Irene Muchoki, the County Chief Officer – Medical services in Nairobi (see photo above) could not hide her excitement and appreciation to LSTM, as she addressed healthcare providers (HCPs). She officially launched a series of healthcare provider (HCP) trainings in EmONC that reached 201 frontline HCPs and 19 trainers in the county.
Following the EmONC training, a county team of 16 experienced healthcare professionals comprising 8 doctors (including 4 OBGY consultants) and 8 midwives continue to support facility-based mentors in strengthening linkages between EmONC and Maternal and Perinatal Death Surveillance and Response (MPDSR), in order to improve MNH quality of care and subsequently mother and child health outcomes.
In December 2023, the county team (including Director of Family Health, County Reproductive Health coordinator, and the County Obstetrician) together with LSTM conducted post-training site visits to six health facilities in Nairobi County. All the health facilities visited demonstrated positive changes in clinical practice building on the knowledge and skills acquired at the EmONC training.
At Mama Lucy Kibaki hospital, a level-5 government facility, the 66-bed capacity maternity wing which delivers between 20-30 babies on a daily basis had almost 60 HCPs undertake the trainings.

The EmONC training was very skills-based. Previously, we used to have Continuous Medical Education (CME) sessions which were mostly theoretical but since the training, we have started conducting structured EmONC mentorship sessions with colleagues in maternity as well as for nursing students on attachment at the hospital ...
Reported the Maternity-in-charge of Mama Lucy Kibaki hospital to the visiting county team.
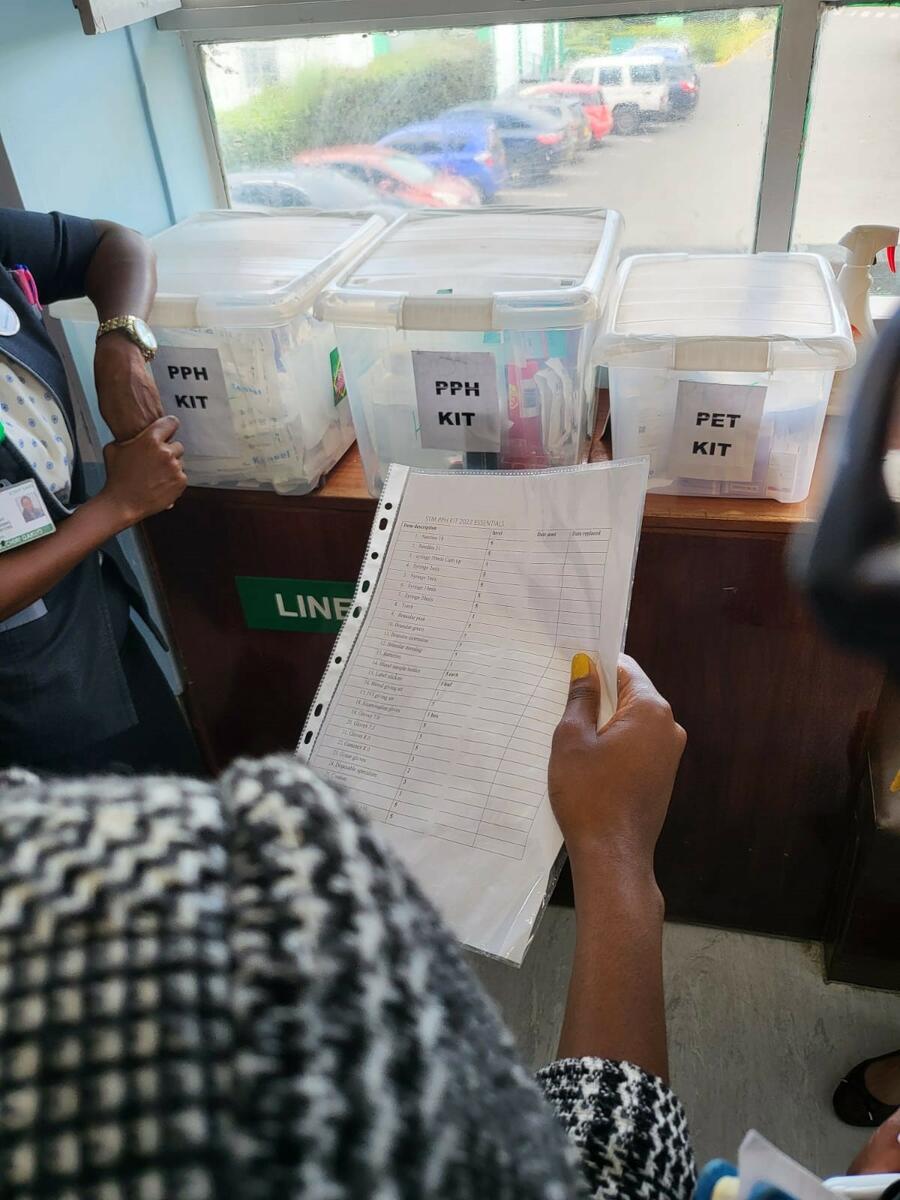
At Mater Misericordiae Hospital a level-5 faith-based facility, following the EmONC training, the maternity team constituted emergency kits for managing Preeclampsia and Postpartum Haemorrhage (PPH).
Having the kits in place ready for use has saved the midwives a lot of time and effort spent in finding the required items to manage patients, which in fact are obstetric emergencies requiring urgent attention ...
reported the Maternity-in-charge to the visiting county team.
A best-practice at the Mater Misericordiae hospital is the ‘mentorship tree’, an organogram the hospital management have designed that links each healthcare provider in maternity to a mentor; and staff duty-shifts are allocated in a way that facilitates frequent interaction between mentees and their respective mentors while going about their tasks.
Other facilities visited include Mbagathi Subcounty hospital, where staff have also constituted emergency trays in maternity, postnatal wards and MCH clinics to improve efficiency and effectiveness in managing obstetric emergencies, since the training. Mutuini Sub County Hospital, St Mary's Mission Hospital and St Francis Community Hospital were also visited by the county team.
Key gaps and challenges observed during the facility visits include overcrowding especially at public-owned health facilities, sometimes having mothers admitted in the hospital share beds makes it difficult to administer certain aspects of quality care. Staff shortages, lack of delivery beds in labour ward that makes child birth and other procedures (e.g. repair of perineal tears) difficult; lack of equipment e.g. NASG[1], Kiwi devices, patient monitors; absence of skills labs and training equipment to facilitate practical sessions during EmONC mentorship, inadequate copies of EmONC manuals and logbooks for especially mentees, inadequate knowledge and skills on how to implement MPDSR activities; etc. ‘SMART’ action plans were jointly developed with each facility to address specific gaps for better service delivery.
Despite the above-mentioned gaps and challenges, post EmONC training, the HCPs have made demonstrable changes in their clinical practices to ensure mothers and newborns receive optimal care within the available resources. These facility visits have been incorporated into the county support-supervision schedule with the county health team committing to address gaps and subsequently improve MNH outcomes in Nairobi.
In a populous urban county, which carries a high burden of maternal deaths in Kenya, “Zero maternal and neonatal deaths” may sound an impractical vision, however consistent EmONC mentorship at health care provider, health facility and county levels could contribute to making this vision a reality in Nairobi.