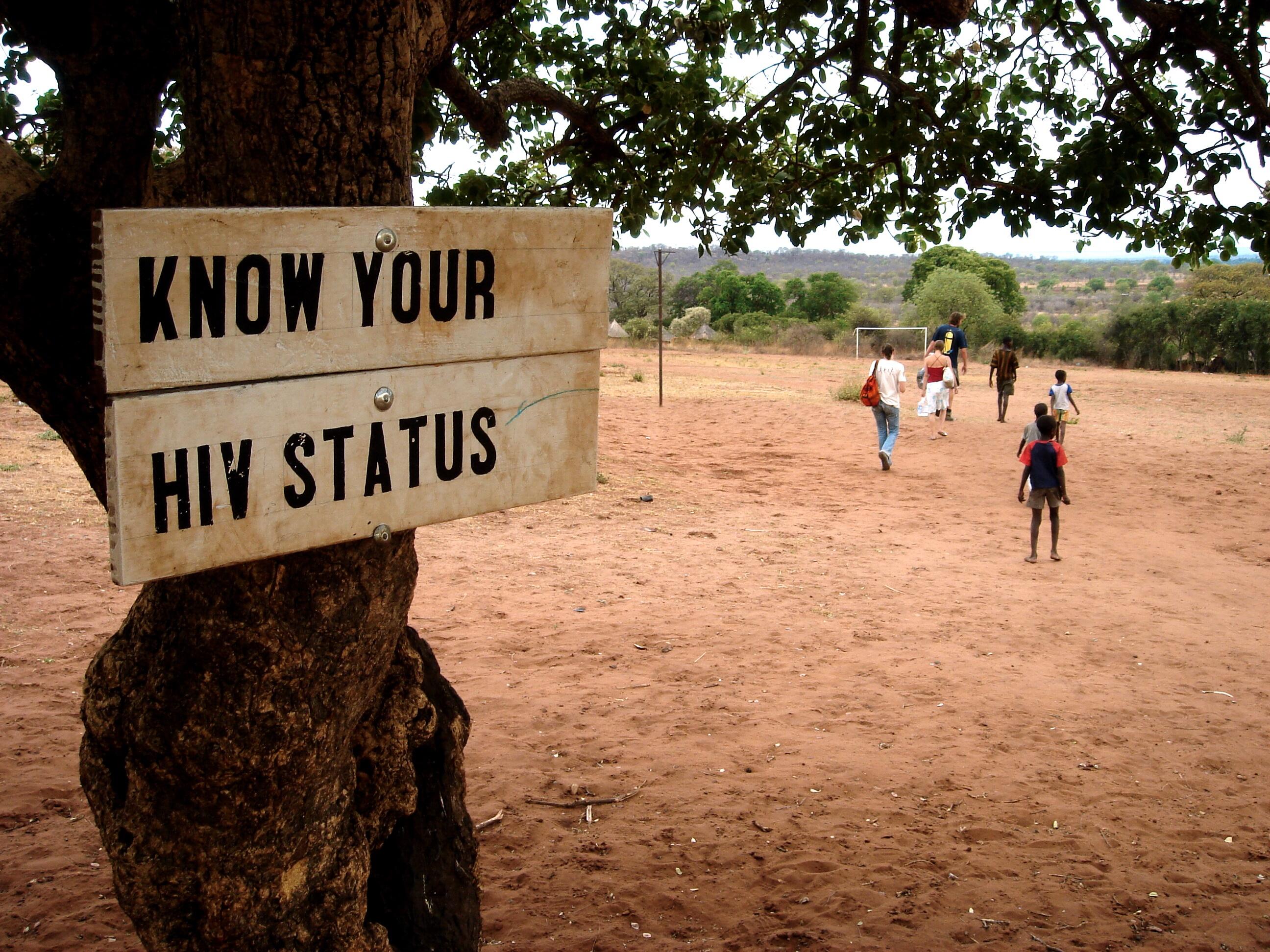
LSTM has developed a successful approach to the rapid scale-up of HIV Testing and Counselling (HTC) services in high prevalence countries, a vital component of the global HIV response. The model combines comprehensive quality assurance with operational research and has led to HTC expansion in mobile, home and facility –based settings. It has also allowed for responsiveness to local needs leading to post rape care services linked to HTC; services for the deaf and HTC for men having sex with men (MSM) and other hidden populations in Africa. The global impact of this model is reflected in WHO policy; Ministry of Health HTC guidelines in numerous countries in Africa; the ongoing work of an indigenous Kenyan NGO and expansion of HTC through community outreach in the UK.
Underpinning research
Through a range of collaborations in Africa, Asia and the UK, LSTM has led research in the development and scale-up of quality assured, complex interventions to increase diagnosis of HIV, prevent transmission and improve HIV outcomes especially in generalised HIV epidemic areas and amongst adolescents and marginalised groups.
HTC services using rapid diagnostic (20 minutes) HIV tests have helped millions of people learn their HIV status, and for those testing positive, learn about options for long term care and treatment.
LSTM conducted a DfID-funded pilot project in 1999 assessing the feasibility, acceptability and cost of integrating these newly available rapid tests into three primary health centres in Kenya. Integration was found to be both acceptable and feasible, to be associated with behaviour change and significantly reduced cost. It represented a significant improvement on previous practice where deferred results led to 47-66% of persons tested not receiving results
Research led to the first published descriptions of translating these pilot studies into the scale-up of HTC services in high prevalence countries, a vital component of the global HIV response.
Qualitative studies in the UK indicated acceptability and feasibility of similar approaches to point of care testing for HTC, although impact data was required before commissioners in the UK would make this part of routine HIV services. LSTM therefore conducted a pilot study in 2009- 2010 in Liverpool using similar training, community entry, supervisory methods and radio interview outreach as done in Kenya. This brief 2009 pilot resulted in 953 tests and 17 new positives diagnosed and linked to care and treatment, an approach that is now funded by commissioners and integrated at the Royal Liverpool University Hospital.
Details of impact
HIV presents a significant health burden in Kenya with an estimated 104,000 infected children and 1,192,000 persons living with HIV infection in 2012. Early treatment has been associated with a 96% reduction in onwards transmission of HIV and theoretical modelling has shown that testing scale-up accompanied by treatment could lead to the eradication of HIV within a decade. LSTM’s research has increased testing, both directly through the changes in policy and systems in Kenya and indirectly through the scalable quality assured services delivered in institutions.
- Health impact
- Policy impact
Kenya
International
UK
For more information on this impact case study including research references; key research grants and sources to corroborate the impact please click here
This impact case study was part of LSTM’s joint submission with University of Liverpool to REF2014.
Global Scale-Up HIV Self Testing: Reaching Vulnerable Populations
The following virtual seminar was delivered on 30 September 2020
Professor Miriam Taegtmeyer and Professor Frances Cowan are key partners in the STAR initiative which aims to stimulate the market for HIV self-test kits through supporting countries in Southern Africa to scale-up self-testing.