The Challenge
In many Kenyan counties, pregnant women first engage with Community Health Promoters before reaching antenatal care (ANC) services at health facilities. But communication gaps between the community and the clinic often mean delays, missed appointments, or duplicated records. With Kenya now aiming for eight ANC contacts during pregnancy, these gaps risk leaving women behind.
The Innovation
Through the C-it DU-it programme, we developed a unique electronic linkage module that connects two government systems:
- eCHIS (electronic community health information system), and
- KenyaEMR (facility-based electronic medical record).
For the first time, referrals can move smoothly and electronically between the community and facility, allowing referrals and follow-ups to be tracked and monitored in real time when systems are online. This innovation is critical because until now, the two systems worked in isolation, leading to duplication, gaps in care, and poor data use. The linkage brings:
- Continuity of care – women can be followed from household to facility.
- Better decision-making – complete, accurate data at all levels.
- Efficiency – reduced duplication and errors.
- Trust and accountability – stronger links between communities and health facilities.
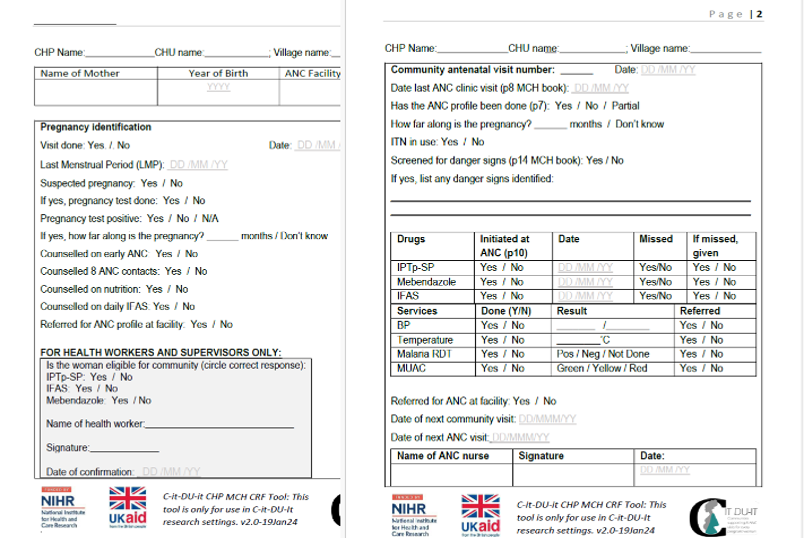
To complement this, we also adapted the widely used Mother–Child Booklet, creating the Community-Enhanced Mother-Child Booklet. Rather than altering its existing content, we simply added a dedicated section for Community Health Promoters to record household visits. This means that facility staff can view a woman’s full history at a glance. Both facility teams and community units report that this small adaptation has transformed coordination, improved trust, and saved time.
The Impact
The adapted Mother-Child Booklet has quickly become more than just a record: it is seen as a silent supervisor, an accountability tool, and even a source of motivation for Community Health Promoters (CHPs). Nurses value being able to see at a glance who the CHP has already visited, while CHPs appreciate that their work is visible and recognized. One CHP explained, “I ask the woman, ‘who is your CHP?’ then I text them. It helps us follow up.”
The Community Household Antenatal Record Tracker (CHART) section has become a practical way of communicating between the community and the clinic. It reduces duplication, ensures timely follow-up, and strengthens collaboration: “The CHART helps you to do the follow up … it is another way of supervision and appreciation.”
While a few challenges remain, such as women living with HIV not always wishing to share their booklet, the overall feedback is overwhelmingly positive. Health workers describe it as simple to use, not burdensome, and a tool that should continue even after the C-it DU-it project ends: “When C-it DU-it leaves, the CRF must remain … it should be adopted nationally!”
Through training and joint support, the CHART has given both CHPs and facility staff a stronger sense of connection, coordination, and purpose. As one CHP put it: “It is a mutisha (motivation).”
The Way Forward
The strong endorsement from both CHPs and facility staff who repeatedly stressed that the CHART “must remain” and “should be adopted nationally” has caught the attention of county health managers. Building on this momentum, there is growing consensus that the adaptation should be scaled beyond the pilot counties.
At the same time, the electronic linkage is opening doors for a new era of seamless data use between communities and clinics, not only for ANC but also for wider maternal, newborn, and child health services.
By “seeing it” (C-it) and “doing it” (DU-it), we are making data work for mothers, babies, and health teams alike.
This research is funded by the NIHR using UK international development funding from the UK Government to support global health research.