
Authors
- Duncan Shikuku (Senior Technical Officer and Associate Fellow of the Higher Education Academy, UK)
- Dr. Charles Ameh (Professor of Global Health – Liverpool School of Tropical Medicine and University of Nairobi (Obstetrics & Gynaecology Department)
Background
The global maternal mortality ration (MMR) in 2020 was estimated at 223 maternal deaths per 100 000 live births, down from 227 in 2015 and from 339 in 2000 – a reduction of one third (34.3%) over the full 20-year period. Despite the reduction, this is still beyond the sustainable development goal (SDG) target 3.1: reduce global MMR to less than 70 maternal deaths per 100 000 live births by 2030. This clearly shows that substantial shifts in focus and investment are needed if the SDG target is to be met. Skilled health personnel (SHP) and emergency obstetric care (EmOC) are global strategies to ending preventable maternal mortalities. The recent State of the World Midwifery Report 2021 indicates that midwives trained to international standards can provide over 90 percent of sexual, maternal, newborn, child and adolescent health. The International Confederation of Midwives (ICM) stipulates the competencies for midwifery practice to accelerate the reduction of maternal and newborn mortality. Liverpool School of Tropical Medicine - Emergency Obstetric and Quality of Care Unit supports interventions aimed at improving the quality of pre-service midwifery education through the Alliance to Improve Midwifery Education (AIME) globally. This is through strengthening global midwifery curricula (and faculty development) to ensure that it aligns with the required ICM competencies and standards encompass the latest scientific evidence and WHO recommendations for midwifery education and practice. Nationally, LSTM supports pre-service and in-service interventions to improve the quality of care and maternal and newborn health outcomes. In line with the International Day of the Midwife 2023 theme “Together again: from evidence to reality,” below is the summary evidence from research and knowledge management and learning to the midwifery interventions supported to accelerate positive trends in maternal and newborn health care in Kenya.
Kenya’s maternal mortality progress
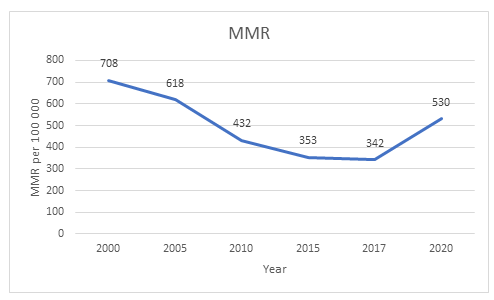
The recent Kenya Demographic and Health Survey 2022 reported marked improvement in births attended by a skilled health personnel over the past two decades from 41% in 2003 to 89% in 2022. Although the skilled birth attendance has increased in Kenya, MMR has not reduced at a similar rate (see figure below). This is potentially due to poor quality of pre-service midwifery education, poor staff retention after in-service EmOC training and challenges with the enabling environment including staff shortages, inadequate supplies and blood products and the impact of the COVID-19 pandemic.
Skilled health personnel strategy
From 2008, Liverpool School of Tropical Medicine (LSTM) in collaboration with the Kenya Ministry of Health and county governments have trained over 11,000 skilled health personnel in emergency obstetrics and newborn care (EmONC) to date. However, a study in five of the supported counties showed that the retention of EmONC trained SHP in the relevant maternity departments was low at 36 percent. For impact, county policies and guidelines on SHP deployment, transfers and retention should be strengthened to optimise the benefits of EmONC training. Through the Johnson & Johnson Foundation support, county leadership in the five counties has been strengthened to manage staff deployment & transfers and counties are using staff training database & commitment to retain SHP in relevant MHH departments for impact. In addition, staff recognition and reward, for motivation to sustain high performance of SHP in maternity departments contributes to the improved quality of care for women and their newborns. Besides, co-creation of EmONC capacity building systems with the counties and MoH that include mentoring, monitoring and regular dissemination, is catalytic in driving health system investments to improve the enabling environment.
Pre-service midwifery education strategy
Improving the quality of and strengthening capacity in midwifery education is a critical component of improving the quality of midwifery care provision and in turn, reduce maternal and newborn mortality. Evidence from implementation research by LSTM in Kenya shows that midwifery educators at university and mid-level training colleges have deficiencies in competencies to deliver a competency-based curriculum integrated with EmONC skills. With donor funding from Foreign, Commonwealth & Development Office (FCDO) and Johnson & Johnson Foundation, LSTM in collaboration with the MoH-led Pre-service Taskforce in Kenya has supported strengthening of pre-service midwifery education and training through several investments: (i) equipping training institutions with obstetric and newborn care equipment, (ii) updated pre-service midwifery curriculum by integrating the life-saving EmONC skills and facilitating online teaching and learning, (iii) strengthened faculty to teach EmONC within the pre-service curriculum and has developed a continuous professional development programme to sustain and improve the competencies of educators in facilitating teaching and learning. These interventions are anchored in the World Health Organization’s seven-step action plan to strengthen quality midwifery education for universal health coverage.
Opportunities for scale-up of interventions
Despite the achievements aimed at strengthening the quality of pre-service midwifery education and practice, there are existing challenges and opportunities for improvement in Kenya at the leadership and policy level to accelerate progress in quality midwifery education and practice. For instance, although the five LSTM-supported counties have signed a commitment to retain EmONC-trained staff within the relevant maternity departments for impact, a national policy on staff deployment/retention for impact would be a bold step towards quality care in all health departments as staff will utilise their training and expertise to better health outcomes. To ensure competent practice, there is need for structured institutional-based mentorship programmes and a mandatory relevant CPD for in-service & pre-service midwifery professionals to regularly update their competencies.
Future plans
Through AIME, LSTM continues to support interventions to improve quality maternal and newborn health services through midwifery by prioritizing curriculum review and update, training, education, and professionalization of midwives anchored on WHO’s midwifery education framework and ICM standards for midwifery education and practice.Interventions are in place to strengthen institutional capacity and faculty development for quality midwifery education and practice through the global Alliance to Improve Midwifery Education. As part of WHO’s seven-step action plan to strengthen midwifery education, there is need to measure impact of midwifery education interventions on MNH outcomes to demonstrate the effectiveness of the implementation to practice.