LSTM was among the first institutions in the world to recognise the importance of studying and understanding the phenomenon of drug resistance. Pioneers such as Professor Warrington Yorke, the first Walter Myers Chair of Parasitology, established in 1929 in vitro cultivation of drug resistant trypanosomes in order to understand the mode of action of new drugs.
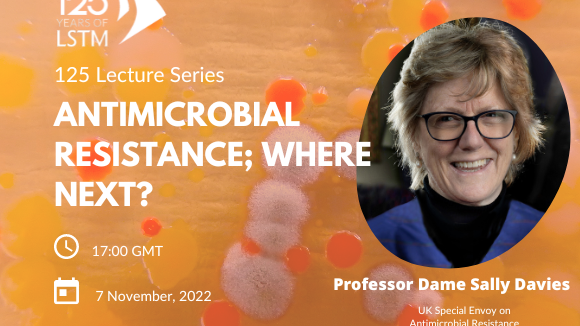
The factors driving the emergence of resistance are complex and multifactorial, and in recognition of this, LSTM has developed a multidisciplinary approach involving the entire research continuum from bench, to patient through to health systems. This has involved cross-disciplinary teams working between laboratory scientists, engineers, mathematical modellers, clinicians, and social scientists.
LSTM's continued commitment to this important area of research is evident from our institutional strategy to use Wellcome Trust ISSF funding to drive appointments and projects in this area.
Understanding principal mechanisms at the molecular level
For many years LSTM has been at the forefront of basic studies into understanding the mechanisms underpinning resistance in malaria, for both the parasite Plasmodium falciparum and the mosquito vector. Members of the Tropical Disease Biology Department have contributed to the discovery of the mechanisms underpinning resistance to a number of antimalarials including chloroquine, antifolates (e.g. Fansidar) and atovaquone. More recently the school is involved in studies attempting to understand the mechanism of action of the artemisinin class of antimalarials, the current last line of defence against the malaria parasite, but for which there are already alarming signs that resistance is emerging in South East Asia which may have catastrophic effects to current malaria elimination initiatives.
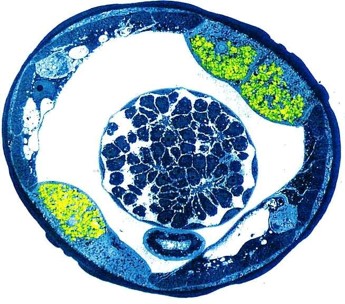
The Department of Vector Biology is leading the search for the molecular mechanisms underpinning resistance to insecticides used in malaria control in the Anopheles mosquitoes that transmit the disease. Using techniques including microarray, RNAseq, association mapping, metabolomics and transgenesis, researchers have identified the major genes responsible for resistance to the key classes of insecticides used to control malaria vectors. This information is being used to identify patterns of cross resistance, develop diagnostics and plan insecticide resistance management programmes. In addition, members of the Vector department are working closely with industry to incorporate this knowledge into the design of new insecticides.
In a recent project, LSTM is driving the Anopheles gambiae 1000 genomes project, led by the Wellcome Trust Sanger Institute, and exploration of this rich data set is providing new clues about the selection process resulting in insecticide resistance
Accelerating the development of new drugs and diagnostics
Drug discovery has been a cornerstone of LSTM activities throughout its history. As early as in 1905 LSTM staff were establishing the effectiveness of the arsenical agent Atoxyl against African Trypanosomiasis. By 1921 the first clinical trials with Suramin were initiated and by 1927 Chemotherapy was established as a core subject by Yorke, Adams and Murgatroyd in LSTM.
The first demonstration of acquired resistance to an antimalarial drug was reported by Fulton and Yorke working with Plamodium knowlesi. Throughout the 40s and 50s LSTM was at the centre of studies to develop chemotherapeutic agents active against, malaria, trypanisomiasis and scabies.
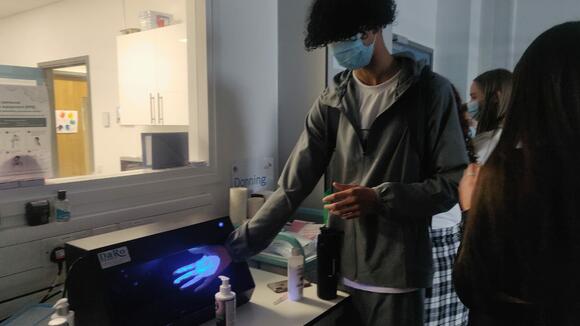
Drug and diagnostic discovery and development remains to this day one of the pillars of LSTM’s activities, taking place in The Research Centre for Drugs and Diagnostics. RCDD regularly works with industry (SMEs and larger organisations), academia and other NGOs to discover, develop and deliver novel therapies against a range of drug resistant pathogens. The Centre has access to state-of-the art laboratories and equipment including Category 3 laboratories, medicinal chemistry laboratories, analytical laboratories, robotic liquid handling and high content imaging platforms. RCDD has an active portfolio in drugs and biologics as well as diagnostics to support the rapid identification and treatment of pathogens in a variety of endemic settings. These activities are commonly delivered in Public Private Partnerships and take advantage of LSTM’s unique cross-disciplinary expertise and global reach which affords access to patient populations and pathways to drug and diagnostic evaluation and implementation in the UK, Africa, Asia and South America, and links to policy makers.
Current drug discovery programmes include the BMGF-funded AWOL consortium, an international academic-industry consortium led by LSTM with the aim to develop a novel anti-Wolbachia based macrofilaricidal drug for the treatment of lymphatic filariasis and onchoceriasis. In addition, there are several pre-clinical projects on-going towards the development of novel therapies against multi-drug resistant malaria parasites and Mycobacterium tuberculosis.
LSTM works the entire diagnostic pipeline from discovery of biomarkers, thorough development and evaluations. We have expertise in the discovery of genomic biomarkers for drug resistance with our bioinformatics group and partner this with assay design and sample preparation, working closely with industrial partners for true product development.
Our Diagnostic Evaluation Platform enables high-quality studies to be performed. Most recently we have set up multi-centre studies to evaluate drug-resistance diagnostics for Tuberculosis including GeneXpert MTB/RIF®, Epistem’s Genedrive® and Hein’s Line Probe Assay®.
The Department of Vector Biology have developed diagnostics for the common mechanisms of insecticide resistance in malaria and dengue vectors. Several of these are now in routine use by national control programmes in disease endemic countries to assist in their insecticide resistance management plans.

LSTM is also playing a critical role in the development of new public health insecticides. We work closely with the Innovative Vector Control Consortium (IVCC) a product development partnership established to accelerate the introduction of new vector control products into the market, by contributing our technical expertise in insecticide resistance mechanisms and the impact of resistance on current control programmes.
LSTM also hosts the Liverpool Insect Testing Establishment (LITE), which provides a professional service to evaluate new insecticides against a wide range of fully characterized insecticide susceptible and resistant strains of mosquitoes.
The AvecNet programme is developing and evaluating new tools to control insecticide resistant malaria. Activities of this consortium, led by LSTM, include a clinical randomized controlled trial of a new type of insecticide treated net in Burkina Faso, evaluation of new products for indoor residual spraying against insecticide resistant populations in the field, measuring both mosquito and human behavioural traits that affect the performance of vector control products, and mapping the regulatory and policy processes that influence the rate of uptake of new malaria prevention tools.
Epidemiology of drug resistance
LSTM operates in over 70 countries, but its largest overseas collaboration is with the Malawi Liverpool Wellcome Trust Clinical Research Programme, where a quality controlled diagnostic microbiology service has been operated for over 15 years. This longitudinal surveillance has enabled us to identify sequential epidemics of multidrug resistant Salmonella bloodstream infection, in the process identifying novel pathotypes of Salmonella, in collaboration with the Wellcome Trust Sanger Institute.
Genetic resistance at a variety of loci is known to exist within soil-transmitted helminths, mutations in beta-tubulin genes being strongly associated with reduced efficacy of benzimidazoles. Tracking the dynamics of these drug-resistant alleles within natural populations and how worms respond to current preventive chemotherapy campaigns is ever more important. The DfID funded programme COUNTDOWN is exploring ways to interface this work within national control programmes.
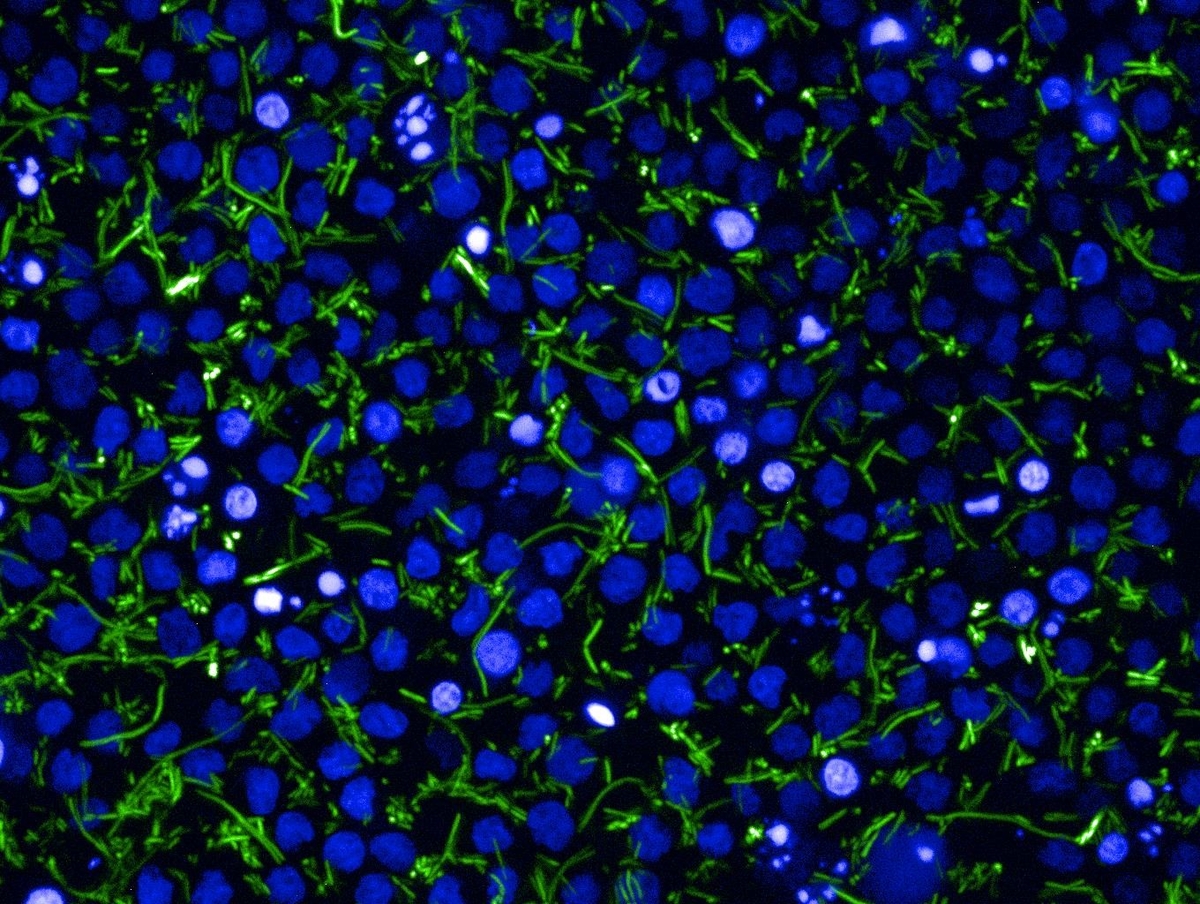
LSTM is working closely with its strong network of partners to understand more about the impact of insecticide resistance on malaria transmission in the field. This complex relationship is being addressed by both detailed laboratory and field studies on the impact of resistance on the behaviour and life time fitness of mosquitoes, modelling studies to predict the impact of resistance, and at the programmatic level by recording the impact of insecticide resistance on the number of malaria cases in the field. At the parasite level, members of the Department of Parasitology have been investigating drug resistance in malaria: its dynamics, how it can be monitored, and how deployment practices can be optimised to mitigate or prevent the spread of resistance. Towards this aim, Dr Hastings currently serves on the WHO Technical Expert Group on “Drug resistance and containment”,
Clinical research
Drug resistance can be mitigated at the clinical level by ensuring that the correct drug doses are being taken for the correct target population. For example many drugs are incorrectly dosed and do not take in to account differences between children and adults or effects due to co-morbidities or drug:drug interactions.
The Department of Parasitology is using PK-PD (pharmacokinetics-pharmacodynamics) methodology to identify safe and effective malaria dosing strategies that are robust to the threats posed by poor patient adherence and by the potential spread of drug resistance.
A novel high-content imaging platform is being used to study the response of intracellular pathogens, e.g. Mycobacterium tuberculosis or Salmonella to drugs, in order to perform PK-PD modelling to select optimal doses that reduce the emergence of resistance.
Effect of human behaviour
Current work at LSTM has documented how a policy of in-patient treatment for recurrent episodes of TB requiring injection therapy is so costly to patients that this acts as a barrier to patients starting and completing the 8 month treatment courses. As a consequence, the Department of Clinical Sciences has piloted community-based injection therapy and demonstrated good adherence to treatment and large reductions in costs to households and the health system.
Health Systems and Policy
Following the refurbishment of the National TB Reference Laboratory in Malawi, LSTM’s Departmetn of Clinical Sciences supported the completion of the a national survey for MDR-TB, documenting, for the first time, current rates of MDR-TB and highlighting the need for changes in the Malawian MDR-TB treatment regimen. The group is responsible for the health economic evaluation of new, shortened regimens for MDR-TB in the STREAM Trial documenting the main drivers of costs of implementing these regimens for patients and health systems. In addition the group have also developed a modelling approach which facilitates country-level decision-making about implementation and scale-up of molecular diagnostics for the detection and management of MDR-TB. This work includes trials of the introduction of these new diagnostics in South Africa, Russia and Brazil.
LSTM is working with the World Health Organization to update guidelines on insecticide resistance monitoring and to evaluate new products designed to be more effective against insecticide resistant populations.
We are also developing and implementing new tools including Insecticide Quantification Kits, Disease Data Management Systems and Serious Gaming into national disease control programmes for malaria and leishamaniasis.